Irritable bowel syndrome (IBS) is a common and chronic gastrointestinal disorder. Symptoms include abdominal pain and cramping accompanied by diarrhea and/or constipation. Estimated to effect 10 to 15% of the population, current drug treatment modalities are fail to relieve symptoms in many patients. There is considerable interest in novel drugs that might more effectively control symptoms while producing limited side effects.
A recent review of treatments for irritable bowel syndrome has been authored by Chang and Talley from the Mayo Clinic. Dr. Chang works in a program identified as Enteric NeuroScience. This designation highlights the importance of neuroscience issues in IBS. Here are my notes from the review:
FDA Approved Drugs in the U.S.
Alosetron (Lotronex)--nerve receptor agonist initially approved for women with IBS and severe diarrhea and then removed from market due to risk of constipation, bowel obstruction and ischemic colitis. Now re-approved but only by prescription from a limited number of physicians participating in monitoring program.
Lubiprostone (Amitiza)--chloride channel activator approved only in women with IBS accompanied by constipation
Nonapproved Drugs
Anticholinergic (antispasmodic)
Scopoloamine also known as hyoscine is an alkaloid drug that has muscarinic antogist effects. Effective in reducing cramping in some IBS patients. May cause dry mouth and blurred vision especially at higher doses.
Peppermint oil: a natural product that appears to have some scientific support for reducing cramping in IBS.
Antidepressants
Tricyclic antidepressants: older antidepressants such as imipramine and doxepin reduce IBS symptoms in some individuals. Effect may be due to anticholinergic effect seen with these older antidepressants.
Selective serotonin re-uptake inhibitors: new selective serotonin re-uptake inhibitors help some with IBS, but also can worsen diarrhea and cramping.
Serotonin norepinephrine re-uptake inhibitors--combine re-uptake blocking of both the serotonin and norepinephrine. Limited study of these agents in IBS but may be promising as they appear to reduce pain in other clinical conditions. Duloxetine (Cymbalta) clinical trial results pending
Drug development targets in IBS
Treatment of visceral hypersensitivity
Kappa-opioid receptor agonists-k-opioid receptor stimulus reduces pain from the gut while not producing constipation characteristic of other opioid
Endocannabinoids- cannabinoids receptors CB1 and CB2 potential targets as activation may reduce pain and hypermotility
Transient receptor potential vanilloid type 1 (TRPV1)-a receptor that is located throughout nervous system and mediates sensation and pain
Beta 3 adrenoreceptor agonists-activation inhibits cholinergic GI contractions and increases release of somatostation. Potentially helpful for inhibiting diarrhea
Neurokinin antagonists-Neurokinin 1 receptor antagonists reduce IBS subjects emotional response to rectosigmoid distention
Centrally acting agents
Dextofisopam-benzodiazepine receptor binding agent that modulates autonomic function
Cholecystokinin (CCK) antagonists
CCK1 antagonism stimulates GI motility and may be helpful in treating IBS associated with constipation
Inflammatory drug targets
Protease-activated receptors-Mast cells release serine proteases that stimulate GI receptors and may play role in visceral hypersensitivty and inflammatory bowel diseases and IBS
A review of clinical trials for IBS at ClinicalTrials.gov shows the following:
Completed trials: duloxetine, mosapride citrate, dextofisopam, crofelemer, itopride HCL, renzapride, asimadoline, alosetron, BMS-562086, mesalazine, St. Johns wort, talnetant
Recruiting: Saccharomyces boulardii, JNJ-27018966, Probaclac, Probiotic
Model of the chemical scopolamine shared under auspices of Creative Commons Attribution-Share Alike 3.0 Unported by author Giorgiogp2
Chang JY, & Talley NJ (2010). Current and emerging therapies in irritable bowel syndrome: from pathophysiology to treatment. Trends in pharmacological sciences, 31 (7), 326-34 PMID: 20554042
Tuesday, 30 November 2010
Monday, 29 November 2010
CBT for Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is a common functional gastrointestinal syndrome characterized by abdominal pain and bowel disturbances (diarrhea and/or constipation). It is estimated to affect 10 to 20% of the population and treatment approaches are often unsatisfactory.
Irritable bowel syndrome can be viewed as a neuroscience problem from several perspectives. Abnormal gastrointestinal motility and hypersensitivity has been identified in IBS--these functions are related to gut nervous system function. The rates of depression and anxiety are high in IBS populations. Pain perception is a central nervous system function. Psychotropic medications appear to be helpful in controlling IBS symptoms in some patients.
An additional neuroscience perspective is the evolving evidence for cognitive behavioral therapy to reduction distress and suffering in IBS. Moss-Morris and colleagues from the UK and New Zealand recently demonstrated the effectiveness of a CBT-self management program for IBS in primary care.
A series of sixty-four primary care patients were randomized to manualized CBT or a treatment as usual control condition. The CBT group completed a seven week program using a manual, one sixty minute face-to-face therapy session and two sixty minute telephone sessions.
The key elements of the CBT program for IBS in primary care included:
1. IBS education--autonomic nervous system interacts with gut, interaction between thoughts, feelings and behaviour and how these can impact stress levels and GI symptoms
2. Assess symptoms and self-monitoring--daily diary of IBS symptoms linked to stress and eating behaviors
3. Managing IBS symptoms--behavioral management of diarrhea or constipation, set goals for managing symptoms
4. Managing unhelpful thoughts-introduction to concept of negative automatic thoughts and their relationship to IBS
5. Personal expectations and activity patterns--perfectionism and other unhelpful personal expectations reviewed
6. Relaxation and stress management-basis stress management and sleep hygiene review--relaxation CD provided
7. Managing flare-ups and the future--probability of flare-ups reviewed, skill use to manage flare-ups and ongoing symptoms emphasized
The key outcome findings for the study:
Symptom relief across all three assessment periods (77% for CBT vs 21% of controls)
At 8 months the CBT group had superior ratings on an IBS symptom severity measure (83% vs 49% of control with clinically significant change)
The authors note that CBT was well accepted with good adherence to treatment. A majority of subjects felt CBT was more effective than any previous treatment they had received. The model is relatively inexpensive compared to a standard 12 to 16 week individual CBT therapy course offered by a psychotherapist.
There is need for identifying ways to incorporate this type of model in the U.S. Adoption of cost-effective treatments is important in this common, chronic disorder associated with significant distress and health care utilization.
Photo of young dik dik from Sudan courtesy of Sarah Yates
Moss-Morris R, McAlpine L, Didsbury LP, & Spence MJ (2010). A randomized controlled trial of a cognitive behavioural therapy-based self-management intervention for irritable bowel syndrome in primary care. Psychological medicine, 40 (1), 85-94 PMID: 19531276
Irritable bowel syndrome can be viewed as a neuroscience problem from several perspectives. Abnormal gastrointestinal motility and hypersensitivity has been identified in IBS--these functions are related to gut nervous system function. The rates of depression and anxiety are high in IBS populations. Pain perception is a central nervous system function. Psychotropic medications appear to be helpful in controlling IBS symptoms in some patients.
An additional neuroscience perspective is the evolving evidence for cognitive behavioral therapy to reduction distress and suffering in IBS. Moss-Morris and colleagues from the UK and New Zealand recently demonstrated the effectiveness of a CBT-self management program for IBS in primary care.
A series of sixty-four primary care patients were randomized to manualized CBT or a treatment as usual control condition. The CBT group completed a seven week program using a manual, one sixty minute face-to-face therapy session and two sixty minute telephone sessions.
The key elements of the CBT program for IBS in primary care included:
1. IBS education--autonomic nervous system interacts with gut, interaction between thoughts, feelings and behaviour and how these can impact stress levels and GI symptoms
2. Assess symptoms and self-monitoring--daily diary of IBS symptoms linked to stress and eating behaviors
3. Managing IBS symptoms--behavioral management of diarrhea or constipation, set goals for managing symptoms
4. Managing unhelpful thoughts-introduction to concept of negative automatic thoughts and their relationship to IBS
5. Personal expectations and activity patterns--perfectionism and other unhelpful personal expectations reviewed
6. Relaxation and stress management-basis stress management and sleep hygiene review--relaxation CD provided
7. Managing flare-ups and the future--probability of flare-ups reviewed, skill use to manage flare-ups and ongoing symptoms emphasized
The key outcome findings for the study:
Symptom relief across all three assessment periods (77% for CBT vs 21% of controls)
At 8 months the CBT group had superior ratings on an IBS symptom severity measure (83% vs 49% of control with clinically significant change)
The authors note that CBT was well accepted with good adherence to treatment. A majority of subjects felt CBT was more effective than any previous treatment they had received. The model is relatively inexpensive compared to a standard 12 to 16 week individual CBT therapy course offered by a psychotherapist.
There is need for identifying ways to incorporate this type of model in the U.S. Adoption of cost-effective treatments is important in this common, chronic disorder associated with significant distress and health care utilization.
Photo of young dik dik from Sudan courtesy of Sarah Yates
Moss-Morris R, McAlpine L, Didsbury LP, & Spence MJ (2010). A randomized controlled trial of a cognitive behavioural therapy-based self-management intervention for irritable bowel syndrome in primary care. Psychological medicine, 40 (1), 85-94 PMID: 19531276
Refined Coconut Oil
It’s funny that with all the information I put out there, I get one question in particular five times for every other question I receive. That question is, “Why do you recommend refined coconut oil?”
I thought it would be good to answer that question once and for all and be able to send a link to people instead of a long-winded response.
Refined coconut oil is not necessarily something I recommend because it is superior to extra virgin coconut oil. It’s not really. However, you must understand the basic qualities of the world’s most highly-concentrated source of saturated fat, and then proceed to get plenty of it in ya.
Because coconut oil is so highly saturated, it is the most stable oil on the planet – meaning, it is the most resilient to heat, light, and air. Whether coconut oil is expeller pressed (refined) like the Tropical Traditions oil I usually buy, or super duper extra virgin is not much of an issue. You could drop a nuclear bomb on a jar of coconut fat and it’s going to come out the other side unharmed. The extra virgin processing really isn’t necessary like it is with seed oils.
Extra virgin coconut oil’s biggest turnoff is its strong taste. Because of its strong taste and odor, its versatility as a cooking oil is greatly reduced. I used to take spoonfuls of extra virgin coconut oil straight, put it in smoothies, and use it to cook a bunch of stuff. At first I didn’t mind the taste, over time I did. I can’t stand the taste now, much less the smell. It’s revolting. The refined oil, however, is odorless and flavorless, and very well could be the most excellent and versatile of all cooking oils. Cooking most of your food in extra virgin coconut oil is gross, but you will automatically cook most of your food in refined coconut oil because it truly is the king of cooking oils.
Extra virgin coconut oil is also far more expensive than refined coconut oil. Usually triple the price. This is money thrown down the toilet for an oil that can fully handle expeller pressing and come out unharmed.
Lastly, many people experience nausea and diarrhea when consuming extra virgin coconut oil, but they have no such symptoms consuming refined coconut oil. I’ve heard this a lot in those who have made the switch.
All those things put together and refined coconut oil is the champ. I never was able to make coconut oil a permanent habit until I made the switch to the refined version. I now use it for deep frying, sautéing, making my beloved homemade French fries, and more – and it is one of the cheapest sources of calories on earth, which is a rare attribute for many “health foods.” The above 5-gallon bucket provides 1,333 calories per dollar, nearly 100 times cheaper than many vegetables.
The main reason for consuming a fair amount of coconut oil is that it helps increase the ratio of saturated to unsaturated fats in your diet. This protects against cellular oxidation and aging, as well as the free radical damage that is neatly tied to most of the degenerative diseases. It is also lower in free radicals by virtue of the fact that it is not damaged by high-heat cooking.
It seems to be capable of improving the immune system response as well, even providing great symptom relief to those suffering from AIDS, potentially due to its ability to increase the production of Mead Acid when displacing polyunsaturated fat, what some believe to be the ultimate solution for the massive Arachidonic Acid pileup seen in modern Westerners (Arachidonic acid, AA, is the substrate for forming many inflammatory molecules in the body associated with nearly all degenerative diseases from asthma to obesity - Mead acid replaces AA when AA is unavailable... read more about AA and why displacing it may yield dramatic health improvements HERE).
Coconut fat is also believed to stimulate the metabolism, which can most likely be attributed to the fact that it is a saturated fat, and not an unsaturated fat – as polyunsaturated fat has a well-understood anti-metabolic property. I think the research illuminated by Ray Peat in this category is very accurate…
“Another cheap food additive, coconut oil, was found to increase feed consumption while slowing weight gain, so it wasn't popular in the meat industry. The highly unsaturated seed oils had the opposite effect, of producing a rapid fattening of the animal, while decreasing feed consumption, so by 1950 corn and soybeans were widely considered to be optimal feeds for maximizing profits in the production of meat animals. It was at this time that the industry found that it could market the liquid oils directly to consumers, as health-promoting foods, without bothering to turn them into solid shortening or margarine. Somehow, few physiologists continued to think about the implications of metabolic slowing, obesity, and the related degenerative diseases.”
-Ray Peat
http://raypeat.com/
If Peat’s writing is a little much for your cranium, there is a great interview with Peat on lipids that you can listen to HERE http://eluv.podbean.com/?s=ray+peat
And coconut oil seems to have an anti-bacterial, anti-viral, and anti-parasitic quality to it as well – all attributes that can probably be linked to the rise in metabolism that coconut oil can trigger.
All this put together, and coconut oil has great potential to assist a population struggling with reduced metabolism, chronic infections, an inflammation epidemic, over-reactive immune systems, and a huge free radical burden.
And there’s hardly a change that is more simple and painless to make for the vast majority of people – replace liquid vegetable oils in your home kitchen with refined coconut oil. Other than your food coming out tasting better, and you feeling better after eating your meals, you won’t even notice making the switch.
For more on saturated fats vs. polyunsaturated fats read THIS FREE EBOOK.
I thought it would be good to answer that question once and for all and be able to send a link to people instead of a long-winded response.
Refined coconut oil is not necessarily something I recommend because it is superior to extra virgin coconut oil. It’s not really. However, you must understand the basic qualities of the world’s most highly-concentrated source of saturated fat, and then proceed to get plenty of it in ya.
Because coconut oil is so highly saturated, it is the most stable oil on the planet – meaning, it is the most resilient to heat, light, and air. Whether coconut oil is expeller pressed (refined) like the Tropical Traditions oil I usually buy, or super duper extra virgin is not much of an issue. You could drop a nuclear bomb on a jar of coconut fat and it’s going to come out the other side unharmed. The extra virgin processing really isn’t necessary like it is with seed oils.
Extra virgin coconut oil’s biggest turnoff is its strong taste. Because of its strong taste and odor, its versatility as a cooking oil is greatly reduced. I used to take spoonfuls of extra virgin coconut oil straight, put it in smoothies, and use it to cook a bunch of stuff. At first I didn’t mind the taste, over time I did. I can’t stand the taste now, much less the smell. It’s revolting. The refined oil, however, is odorless and flavorless, and very well could be the most excellent and versatile of all cooking oils. Cooking most of your food in extra virgin coconut oil is gross, but you will automatically cook most of your food in refined coconut oil because it truly is the king of cooking oils.
Extra virgin coconut oil is also far more expensive than refined coconut oil. Usually triple the price. This is money thrown down the toilet for an oil that can fully handle expeller pressing and come out unharmed.
Lastly, many people experience nausea and diarrhea when consuming extra virgin coconut oil, but they have no such symptoms consuming refined coconut oil. I’ve heard this a lot in those who have made the switch.
All those things put together and refined coconut oil is the champ. I never was able to make coconut oil a permanent habit until I made the switch to the refined version. I now use it for deep frying, sautéing, making my beloved homemade French fries, and more – and it is one of the cheapest sources of calories on earth, which is a rare attribute for many “health foods.” The above 5-gallon bucket provides 1,333 calories per dollar, nearly 100 times cheaper than many vegetables.
The main reason for consuming a fair amount of coconut oil is that it helps increase the ratio of saturated to unsaturated fats in your diet. This protects against cellular oxidation and aging, as well as the free radical damage that is neatly tied to most of the degenerative diseases. It is also lower in free radicals by virtue of the fact that it is not damaged by high-heat cooking.
It seems to be capable of improving the immune system response as well, even providing great symptom relief to those suffering from AIDS, potentially due to its ability to increase the production of Mead Acid when displacing polyunsaturated fat, what some believe to be the ultimate solution for the massive Arachidonic Acid pileup seen in modern Westerners (Arachidonic acid, AA, is the substrate for forming many inflammatory molecules in the body associated with nearly all degenerative diseases from asthma to obesity - Mead acid replaces AA when AA is unavailable... read more about AA and why displacing it may yield dramatic health improvements HERE).
Coconut fat is also believed to stimulate the metabolism, which can most likely be attributed to the fact that it is a saturated fat, and not an unsaturated fat – as polyunsaturated fat has a well-understood anti-metabolic property. I think the research illuminated by Ray Peat in this category is very accurate…
“Another cheap food additive, coconut oil, was found to increase feed consumption while slowing weight gain, so it wasn't popular in the meat industry. The highly unsaturated seed oils had the opposite effect, of producing a rapid fattening of the animal, while decreasing feed consumption, so by 1950 corn and soybeans were widely considered to be optimal feeds for maximizing profits in the production of meat animals. It was at this time that the industry found that it could market the liquid oils directly to consumers, as health-promoting foods, without bothering to turn them into solid shortening or margarine. Somehow, few physiologists continued to think about the implications of metabolic slowing, obesity, and the related degenerative diseases.”
-Ray Peat
http://raypeat.com/
If Peat’s writing is a little much for your cranium, there is a great interview with Peat on lipids that you can listen to HERE http://eluv.podbean.com/?s=ray+peat
And coconut oil seems to have an anti-bacterial, anti-viral, and anti-parasitic quality to it as well – all attributes that can probably be linked to the rise in metabolism that coconut oil can trigger.
All this put together, and coconut oil has great potential to assist a population struggling with reduced metabolism, chronic infections, an inflammation epidemic, over-reactive immune systems, and a huge free radical burden.
And there’s hardly a change that is more simple and painless to make for the vast majority of people – replace liquid vegetable oils in your home kitchen with refined coconut oil. Other than your food coming out tasting better, and you feeling better after eating your meals, you won’t even notice making the switch.
For more on saturated fats vs. polyunsaturated fats read THIS FREE EBOOK.
Sunday, 28 November 2010
Imaging Theory of Mind Development: TED Saxe Presentation
Theory of Mind relates to the development of an ability to understand the thoughts and emotions of others. fMRI has provided significant insight into the brain region (right parietal-temporal junction) associated with this ability. Dr. Rebecca Saxe from MIT has been a leader in this research. Posted above is her TED talk related to her research--it is about 16 minutes. Posted below are my notes on the presentation:
- As scientist I am interested in how it's so easy to understand what is on other minds.
- Humans have an amazing capacity to understand what's on the minds of others.
- The brain's has a special region dedicated to this function
- Right temporal parietal junction (RPTJ)
- This area has no other major function, it is specific for reading others thoughts
- Children take a long time to develop this skill
- Between ages 3 and 5they begin to understand others can have thoughts different than their own
- Video presented that demonstration of testing this skill in children
- Understanding what is on other people's mind important for moral development
- fMRI studies allow understanding how this brain region develops--from less to much more specialized
- Even adults vary in their ability to understand the thoughts of others
- Video demonstrating testing this skill in adults
- fMRI imaging in adults shows variability in activation of RPTJ with probe
- The function of this area of the brain can modified using transcutaneous magnetic stimulation (rTMS)
- Applying rTMS to the RPTJ modifies level of rating blame
- Q and A period
- Saxe notes the potential misuse of this research and technology
- There has been interest from the Department of Defense in her work
Dr. Saxe's lab for publication list and more information is here.
Saxe RR, Whitfield-Gabrieli S, Scholz J, & Pelphrey KA (2009). Brain regions for perceiving and reasoning about other people in school-aged children. Child development, 80 (4), 1197-209 PMID: 19630902
Saturday, 27 November 2010
Free Vegetarian Starter Kit Booklet
 |
| Physicians Committee for Responsible Medicine |
PCRM Free Vegetarian Starter Kit
Below is also a link to a 12 minute video "Opening the Doors to Compassion" produced by PRCM as well. This video talks about how an aggressive plant-based diet is the ideal intervention to reverse serious health conditions. The video states that children are in the worse shape of any generation we have ever had. One of the most important things PCRM is doing right now is campaigning for better foods in our public schools. Colon cancer risk starts early. Even small amounts of processed meats can lead to adult cancers. PCRM educates members of Congress by sending qualified & informed doctors. PCRM is a nonprofit organization of doctors and others promoting preventive medicine, recommends a quality plant-based diet for the treatment and prevention of many health conditions.
Some of the world's populations are known to have extraordinary long, healthy and happy lives. Disease is virtually unknown, even in the oldest persons. Studies have shown that their exceptional health is largely attributed to low-calorie, plant-based, whole foods diets. Genetics are ruled out as a significant factor – when they are exposed to Western-style diets they quickly develop the same diseases common to Westerners.
PCRM is working to educate people away from their old way of thinking and the bad science. Watch the video below and check out their entire website. http://www.pcrm.org/about/index.html
The Epidemiology of Trauma in PTSD-II
In a previous post, I looked at the varieties of traumatic experiences and their risk of inducing PTSD in men and women. Another aspect of the epidemiology of PTSD is a more basic look at the overall prevalence of exposure to individual traumatic experiences.
There has been significant discussion and research to define the trauma severity required to increase risk of a PTSD response. Early studies tended to have a lower threshold for severity. They included not only a personal experience of trauma but also learning that a friend or family member had experienced trauma. More recent research has required a more direct personal experience for the traumatic experience.
Using an earlier, less restrictive definition, up to ninety percent of survey population reported at least one trauma significant enough for PTSD. The most prevalent traumatic experiences (1996 Detroit area survey)
1. Sudden unexpecte death of a close friend or relative (60%)
2. Learned close friend/relative was seriously injured in a motor vehicle crash (39%)
3. Learned that a close friend/relative was raped or sexually assaulted (33%)
4. Witnessed someone being killed or seriously injured (29%)
5. Personal serious car or motor vehicle crash (28%)
The WHO international study of trauma used a more restrictive list of serious traumatic events and found the prevalence rates for lifetime trauma ranged between 2 and 31%. The most common traumas reported among those with a traumatic experience were:
1. Death of a loved one (31%)
2. Witness to violence (22%)
3. Interpersonal violence (19%)
4. Accidents (18%)
5. Exposure to war (16%)
6. Trauma to a loved one (13%)
Look forward to additional description of the WHO survey of prevalence and patterns of trauma exposure throughout the world.
Photo of Kenyan Zebra Courtesy of Sarah Yates
Breslau, N. (1998). Trauma and Posttraumatic Stress Disorder in the Community: The 1996 Detroit Area Survey of Trauma Archives of General Psychiatry, 55 (7), 626-632 DOI: 10.1001/archpsyc.55.7.626
Stein DJ, Chiu WT, Hwang I, Kessler RC, Sampson N, Alonso J, Borges G, Bromet E, Bruffaerts R, de Girolamo G, Florescu S, Gureje O, He Y, Kovess-Masfety V, Levinson D, Matschinger H, Mneimneh Z, Nakamura Y, Ormel J, Posada-Villa J, Sagar R, Scott KM, Tomov T, Viana MC, Williams DR, & Nock MK (2010). Cross-national analysis of the associations between traumatic events and suicidal behavior: findings from the WHO World Mental Health Surveys. PloS one, 5 (5) PMID: 20485530
There has been significant discussion and research to define the trauma severity required to increase risk of a PTSD response. Early studies tended to have a lower threshold for severity. They included not only a personal experience of trauma but also learning that a friend or family member had experienced trauma. More recent research has required a more direct personal experience for the traumatic experience.
Using an earlier, less restrictive definition, up to ninety percent of survey population reported at least one trauma significant enough for PTSD. The most prevalent traumatic experiences (1996 Detroit area survey)
1. Sudden unexpecte death of a close friend or relative (60%)
2. Learned close friend/relative was seriously injured in a motor vehicle crash (39%)
3. Learned that a close friend/relative was raped or sexually assaulted (33%)
4. Witnessed someone being killed or seriously injured (29%)
5. Personal serious car or motor vehicle crash (28%)
The WHO international study of trauma used a more restrictive list of serious traumatic events and found the prevalence rates for lifetime trauma ranged between 2 and 31%. The most common traumas reported among those with a traumatic experience were:
1. Death of a loved one (31%)
2. Witness to violence (22%)
3. Interpersonal violence (19%)
4. Accidents (18%)
5. Exposure to war (16%)
6. Trauma to a loved one (13%)
Look forward to additional description of the WHO survey of prevalence and patterns of trauma exposure throughout the world.
Photo of Kenyan Zebra Courtesy of Sarah Yates
Breslau, N. (1998). Trauma and Posttraumatic Stress Disorder in the Community: The 1996 Detroit Area Survey of Trauma Archives of General Psychiatry, 55 (7), 626-632 DOI: 10.1001/archpsyc.55.7.626
Stein DJ, Chiu WT, Hwang I, Kessler RC, Sampson N, Alonso J, Borges G, Bromet E, Bruffaerts R, de Girolamo G, Florescu S, Gureje O, He Y, Kovess-Masfety V, Levinson D, Matschinger H, Mneimneh Z, Nakamura Y, Ormel J, Posada-Villa J, Sagar R, Scott KM, Tomov T, Viana MC, Williams DR, & Nock MK (2010). Cross-national analysis of the associations between traumatic events and suicidal behavior: findings from the WHO World Mental Health Surveys. PloS one, 5 (5) PMID: 20485530
Friday, 26 November 2010
The Epidemiology of Trauma in PTSD
PTSD represents a pathological response to a serious trauma. The evolution of the diagnostic criteria for PTSD has included a broadening of the types of trauma exposures felt sufficient to trigger PTSD. The original criteria included combat, concentration camp confinement, natural disaster, rape or physical assault. The current DSM-IV criteria for trauma require that "the person experienced, witnessed or was confronted with an event(s) that involved actual or threatened death or serious injury or a threat to the physical integrity of self or others"
Naomi Breslau from the Michigan State summarized the current state of knowledge regarding the epidemiology of trauma and PTSD--much of which she has been a key research leader. With the expanded trauma trigger definition, it is estimated approximately 40 to 80% of the U.S. population have experienced one of these traumas. General population surveys of PTSD complement our knowledge of PTSD outside military personnel.
Only a minority of trauma exposures appear to result in PTSD. Women appear more vulnerable to a PTSD response than men. Here is the estimated highest risk traumas for women (% of individuals experiencing the trauma who develop PTSD):
Women
In addition to female gender, presence of a prior childhood anxiety disorder appears to increase risk. Higher IQ (>115) appears to provide some protective effect.
Prevention of PTSD starts with public health efforts to reduce violent crime and the frequency of severe trauma exposure in the population. Military service related trauma is also a key area for prevention and early intervention. Secondary prevention efforts include identifying those exposed to serious trauma, assessing for high risk for PTSD following this trauma and early therapy or pharmacologic intervention.
Photo of male lion in Kenya courtesy of Sarah Yates
Breslau N (2009). The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma, violence & abuse, 10 (3), 198-210 PMID: 19406860
Naomi Breslau from the Michigan State summarized the current state of knowledge regarding the epidemiology of trauma and PTSD--much of which she has been a key research leader. With the expanded trauma trigger definition, it is estimated approximately 40 to 80% of the U.S. population have experienced one of these traumas. General population surveys of PTSD complement our knowledge of PTSD outside military personnel.
Only a minority of trauma exposures appear to result in PTSD. Women appear more vulnerable to a PTSD response than men. Here is the estimated highest risk traumas for women (% of individuals experiencing the trauma who develop PTSD):
Women
- Held captured/tortured (78%)
- Severe physical assault with injury (56%)
- Rape (49%)
- Lesser assault (36%)
- Serious accident (28%)
- Sexual assault other than rape (24%)
- Shot or stabbed (18%)
- Child life threatening illness (18%)
- Sexual assault (16%)
- Sudden, unexpected death of relative or friend (13%)
- Witnessing a killing/serious injury (9%)
In addition to female gender, presence of a prior childhood anxiety disorder appears to increase risk. Higher IQ (>115) appears to provide some protective effect.
Prevention of PTSD starts with public health efforts to reduce violent crime and the frequency of severe trauma exposure in the population. Military service related trauma is also a key area for prevention and early intervention. Secondary prevention efforts include identifying those exposed to serious trauma, assessing for high risk for PTSD following this trauma and early therapy or pharmacologic intervention.
Photo of male lion in Kenya courtesy of Sarah Yates
Wednesday, 24 November 2010
Harvest Pot Pies
Happy Thanksgiving! I made these delicious Harvest Pot Pies last night and we all loved them. The recipe makes 8 individual servings. This would be a wonderful main dish. I made my own crust from 100% whole wheat flour, but you can buy a puff pastry and use it for convenience. Make ahead directions are also included. You can create this dish up to 2 days before Thanksgiving and put it together at the last minute. Enjoy!!
Harvest Pot Pie
Printable Recipe
Serves 8
2 tbsp. olive oil
12 oz. button mushrooms, sliced
1 medium onion, chopped (1 cups)
3 stalks celery, diced (about 1 cup)
3 cloves garlic, minced (1 tbsp.)
1 tbsp. chopped fresh thyme
1/2 cup vegetable broth with 1 tsp. apple cider vinegar
1 lbs. butternut squash, cubed
5 small red potatoes, sliced
1/2 lb. green beans, halved
2 cups fresh or frozen corn kernels
3 tbsp. arrowroot powder
5 cups vegetable broth
1 17.3 oz. pkg. frozen puff pastry (2 sheets), thawed (I made my own whole wheat pastry)
1. Heat oil in pot over medium-low heat. Add mushrooms, onion, celery, garlic and thyme. Cover, and cook 10 minutes, stirring occassionally. Uncover, increase heat to medium, and cook 5 minutes more, or until mushrooms begin to brown. Add 1/2 cup broth with apple cider vinegar and simmer 2 minutes, or until liquid evaporates.
2. Add squash, potatoes, green beans, corn and 5 cups water. Cover, and simmer 7 minutes.
3 Whisk arrowroot with 1/2 cup liquid from vegetable mixture. Stir into vegetables. Simmer 2 minute, or until thickened. If making ahead, cool, and refrigerate up to 2 days.
4. Preheat oven to 425 F. Coat 2 baking sheets with cooking spray. Cut 4 circles from one puff pastry sheet. Repeat with remaining sheet. Cut 1 inch hole in center of each circle (I used a lid from my Olive Oil). Cut leaves from dough scraps, then chill tops and leaves 15 minutes. Adhere leaves to tops by brushing with water. Bake 15 minutes, or until brown and puffy. Store cooled tops up to 2 days in airtight container if making ahead.
5. Reheat filling, and warm tops in oven, if needed. Ladle filling into small pie dishes or ramekins. Top with crusts, and serve. Garnish with fresh thyme.
Harvest Pot Pie
Printable Recipe
Serves 8
2 tbsp. olive oil
12 oz. button mushrooms, sliced
1 medium onion, chopped (1 cups)
3 stalks celery, diced (about 1 cup)
3 cloves garlic, minced (1 tbsp.)
1 tbsp. chopped fresh thyme
1/2 cup vegetable broth with 1 tsp. apple cider vinegar
1 lbs. butternut squash, cubed
5 small red potatoes, sliced
1/2 lb. green beans, halved
2 cups fresh or frozen corn kernels
3 tbsp. arrowroot powder
5 cups vegetable broth
1 17.3 oz. pkg. frozen puff pastry (2 sheets), thawed (I made my own whole wheat pastry)
1. Heat oil in pot over medium-low heat. Add mushrooms, onion, celery, garlic and thyme. Cover, and cook 10 minutes, stirring occassionally. Uncover, increase heat to medium, and cook 5 minutes more, or until mushrooms begin to brown. Add 1/2 cup broth with apple cider vinegar and simmer 2 minutes, or until liquid evaporates.
2. Add squash, potatoes, green beans, corn and 5 cups water. Cover, and simmer 7 minutes.
3 Whisk arrowroot with 1/2 cup liquid from vegetable mixture. Stir into vegetables. Simmer 2 minute, or until thickened. If making ahead, cool, and refrigerate up to 2 days.
4. Preheat oven to 425 F. Coat 2 baking sheets with cooking spray. Cut 4 circles from one puff pastry sheet. Repeat with remaining sheet. Cut 1 inch hole in center of each circle (I used a lid from my Olive Oil). Cut leaves from dough scraps, then chill tops and leaves 15 minutes. Adhere leaves to tops by brushing with water. Bake 15 minutes, or until brown and puffy. Store cooled tops up to 2 days in airtight container if making ahead.
5. Reheat filling, and warm tops in oven, if needed. Ladle filling into small pie dishes or ramekins. Top with crusts, and serve. Garnish with fresh thyme.
 |
| The Health Seeker's Kitchen |
Tuesday, 23 November 2010
Drug Development for Cognitive Enhancement
 |
| AMPA (α-amino-3-hydroxyl-5-methyl-4-isoxazole-propionate) |
Cognitive enhancement does not replace other methods of cognitive performance. There is no substitute for repetitive practice and learning content through reading, writing, speaking and physical activity. Cognitive enhancement looks to maximize performance without serious adverse effects risk. The development of drugs and model molecules related to basic brain is expanding.
This is really not a new area as man has been using dietary aids to enhance cognition for thousands of years. Perhaps the best, but not the only, example of this is use of caffeine. Caffeine can increase performance on a number of tests of cognitive function as well as extend the duration of time for productive activity.
Cognitive enhancement candidate drugs include extension of drug used in attention-deficit hyperactivity disorder (ADHD) as well as drugs designed to reduce the rate of cognitive decline in Alzheimer's disease and other dementias. This class of pharmacology has been label the nootropic drugs. de Jongh and colleagues from Utrecht University in the Netherlands recently summarized current and future targets for enhancing cognition. Here is the listing of drugs from their review:
Currently available enhancers
Donepezil-an anticholinesterase inhibitor indicated for Alzheimer's disease with evidence of improved flight simulator performance after training older pilots
Modafanil-seen as a wakefulness enhancer with FDA approval for those shift work sleep disorder. Effective at extending helicopter pilot performance effectiveness up to 36 continuous hours.
Dopamine agonists (d-amphetamine, bromocriptine, pergolide)-appears to improve working memory, particularly for those with memory problems or the COMT genotype val/val associated with reduced prefrontal dopamine levels
Guanfacine- Alpha 2 adrenergic receptor agonist approved for ADHD in the U.S. Inconsistent findings of improved memory and executive function
Methylphenidate--Improves prefrontal cortical function in rodents but ineffective for age related cognitive decline found in older human research volunteers
Future targets
AMPA receptors-Ampakines are drugs that enhance fast excitatory neurotransmission by modulating AMPA (α-amino-3-hydroxyl-5-methyl-4-isoxazole-propionate see diagram above)-type glutamate receptors--effective in improving memory and performance after sleep deprivation in monkeys. Also effective improving memory in healthy elderly (65-75 years of age) human study.
NMDA receptors-D-cycloserine, a partial agonist at the NMDA receptor enhances memory and has been effective in increasing the speed of response to psychotherapy as noted in previous Brain Post commentary here.
CREB (cAMP response element binding protein)-cAMP response element protein a crucial compound in long-term memory formation. Has problems with adverse effects (anxiety and depression) outside of brain amygdala.
Mood and pro-social behavior
Antidepressants-may have some ability to increase social behaviors in those without depression, also felt to improve "hassle tolerance"
Oxytocin-increases pro-social behaviors such as pair bonding and maternal care. Leads to increased trust in others in social game simulations.
Research in this area carriers some significant ethical challenges that will need discussion and consideration. Nevertheless, look for additional research into "nootropic" drug development.
DEJONGH, R., BOLT, I., SCHERMER, M., & OLIVIER, B. (2008). Botox for the brain: enhancement of cognition, mood and pro-social behavior and blunting of unwanted memories Neuroscience & Biobehavioral Reviews, 32 (4), 760-776 DOI: 10.1016/j.neubiorev.2007.12.001
Monday, 22 November 2010
Paula Owens: The Power of 4
First things first, Chris Sandel mentioned in the last post is doing a series on RRARF that you guys might be interested in... http://www.seven-health.com/blog/
To find out more about RRARF, which stands for Rehabilitative Rest and Aggressive Re-Feeding, please read THIS FREE EBOOK.
Now let's get down to bidniss. After doing my book review of Rachel Cosgrove’s The Female Body Breakthrough, I was immediately contacted by Paula Owens and asked if I would review her book as well. Well of course I will! Send me that badboy and I’ll review it right away. And so I am.
Anyway, this is not some big promo for Paula Owens and her book. Like with the Cosgrove book I call ‘em like I see ‘em and am not in the business of making friends or creating alliances. Here is my most honest and level-headed review of Paula Owens and her Power of 4, which refers to the power of nutrition, lifestyle, exercise, and supplements.
Overall, the book gives the reader more or less the right information. Right away I could tell that Owens has been highly influenced by Diana Schwarzbein, Paul Chek, Charles Poliquin and others that are pretty knowledgeable. These authors all generally believe that health is something that is hormonally determined, and that the best way to optimize the hormonal environment is through quality nutrition, a low-stress lifestyle with the right attitude, “smart” exercise meaning a preference for resistance training over endurance exercise, and supplements if needed.
With a foundation like that, the information in the book is more or less solid and can only stray so far from guidelines of the highest importance.
Of course the book has a pronounced low-carb bias due to such influences, which in the modern world probably does tend to outperform high-carb diets knowing that your average American receives 1,100 daily calories from a combined total of refined sweeteners and white flour. A low-carb diet eliminates this catastrophic problem, and is automatically superior – especially in the short-term. But there were definitely some one-liners in there about “too many carbohydrates” as if carbohydrates were somehow the enemy. If I’ve discovered anything about carbohydrates it’s that shunning carbohydrates in general simply can’t compete with replacing “bad” carbohydrates with “good” carbohydrates – which I view as more of an antidote to the problems caused by excess refined carbohydrate consumption.
But Owens is still clearly not an extremist by any stretch, and doesn’t deserve to be raked over any coals for her low-carb bias as it is VERY slight.
Rather, Owens should be truly commended for her excellent exercise information. Owens has several personal training certificates and it’s more than obvious that this is her area of expertise. Just as with Cosgrove, the exercise segment is by far the highlight. Some quotes from her chapter on reducing “LSD,” or long, slow, distance training, are truly legendary. For creating an optimal hormonal environment for both physique enhancement, metabolism, and functional longevity, I couldn’t agree more that short, hard training and resistance exercise and avoidance of LSD is the ticket. Paula’s ripped female figure is strong testimony to that.
p. 193
"One must exercise for long duration and often in order to burn any amount of fat with LSD. This is how long distance runners maintain their slim physiques. However, when a runner sustains an injury and is unable to train their metabolism spirals down. This leads to increased body fat over time."
This has been my response to endurance exercise time and time and time and time and time again. Only when it exceeds 20 hours per week is the calorie burn so high that fat has no choice but to leave your body. This exercise is very hard on the body, it causes muscle loss and a huge drop in metabolism (sends my basal temp. to the low-96’s), and results in a higher ratio of body fat to lean mass the MOMENT that you stop doing it – which you likely will due to injury, illness, or burnout.
p. 197
"LSD exercise is problematic because it causes cortisol to rise unopposed by the growth-promoting hormones, testosterone and growth hormone. This creates a physical stress response to your entire body. Prolonged release of cortisol, whether from long-term physical mental, or emotional stress, or the wrong kind of exercise, atrophies your muscles, nerves and brain cells. This may explain why standard aerobic exercise is not effective for optimal body composition and why marathon runners exhibit frail bodies devoid of muscle. The duration - not the intensity - of the exercise is the most significant issue in regards to cortisol. Chronic over-secretion of cortisol causes a weakened immune system, a decrease in lean muscle, hair loss, thinning skin, infertility, inability to grow nails and a decrease in concentration and memory. Excess cortisol kills brain cells, including those in the hippocampus, where the brain processes emotions. Excessive cortisol production can also deplete serotonin levels causing depression."
This quote is pure genius, and after the Thanksgiving holiday I hope we get a chance to dive straight into the diametrically-opposed functions of cortisol and testosterone – and how this is a prime determinant of how you age, your body composition, your immune system, athletic ability, and more. BTW Scott Abel's blog post on holiday eating is out of this world. Read it HERE.
So yes, overall Paula’s book is great. The exercise segment is remarkable and spot on. Now time for some negative criticisms…
Owens continually comes up with various lists of things to do in each category. While I wouldn’t disagree with many of her bulleted items in terms of say, their validity, I think it is a huge error to give your average person multiple lists of almost jaw-dropping length to focus on for health. Her list on lifestyle, for example, would be much better if she picked the top 4 most important things for people to focus on. Instead, the list, I kid you not, contains over 50 To-do’s, and includes nebulous and distracting things like:
“Refrain from judgment” and “Journal your thoughts.”
Her list in the nutrition category is even longer and puts the same emphasis, due to the nature of her lengthy bulleted lists, on including “more green drinks to create alkalinity” and eliminating “refined sugar.” Clearly there needs to be a little more prioritization going on there.
Of course, most of her bulleted items aren’t even discussed in detail. Several things that you are supposed to do would require a book on why you should do that. Lists of “do this, don’t do that” without any explanation or reasoning as to why doesn’t sit well with me, and I can’t see such things making any kind of impact on a real person in the real world. Rather it obscures the few basic things that really do make a difference with a bunch of nebulous, paranoid, distracting stuff that really doesn’t.
While Paula may have some powerful know how and knowledge that she is eager to share, her strategy for writing this book was not very well thought out. She shared far too much with too little to back it up.
There were also some unbelievably odd and off-base statements made here and there. They really threw me off. For example:
p. 40
“Reducing your intake of sugar and refined grains, which are omega-6 fatty acids, will result in decreased triglycerides.”
What the huh?
p. 41
“Grain-fed beef, refined cereals and vegetable oils such as sunflower, safflower, corn and soybean are foods high in omega-6.”
Grain-fed beef and refined cereals are not high in omega 6. In fact, by weight, walnuts (something Paula likes and advocates eating even though she is anti omega 6), contain 116 times more omega 6 than grain fed ground beef sirloin (90% lean). And refined cereals have a lot LESS omega 6 than unrefined cereals.
Conclusion:
Overall, I get a great vibe from Paula. There’s no question that if you are a woman (or man) living near the Phoenix area where Paula resides and looking for someone to help you improve your health and get a body that you never thought possible, Paula is the FIRST person to call. I have no doubts that her 21-Day Program is a great place for anyone to start when it comes to improving their health and body composition.
The book itself is full of great information, clouded by Mercola-fication of having 327 things to address when getting healthy instead of something more realistic, and just not that well written (typical of many great minds in the fitness field who attempt to write books). I would never discourage anyone from reading it though, as all of it is on the right track and there’s no doubt that the lives of many will be positively influenced by the gems that reside in The Power of 4. Thank you Paula, for putting it out into the world and overflowing with your passion for health. There are many in need of guidance out there, and I can only assume from what I know of you thus far that you are one of the world’s best. Keep up the good work. And Paula, you are totally hot (like Gwyneth Paltrow without the macrobiotics-induced osteopenia). You don't need your dog in the picture to make you look good :) More from Paula at www.paulaowens.com
To find out more about RRARF, which stands for Rehabilitative Rest and Aggressive Re-Feeding, please read THIS FREE EBOOK.
Now let's get down to bidniss. After doing my book review of Rachel Cosgrove’s The Female Body Breakthrough, I was immediately contacted by Paula Owens and asked if I would review her book as well. Well of course I will! Send me that badboy and I’ll review it right away. And so I am.
Anyway, this is not some big promo for Paula Owens and her book. Like with the Cosgrove book I call ‘em like I see ‘em and am not in the business of making friends or creating alliances. Here is my most honest and level-headed review of Paula Owens and her Power of 4, which refers to the power of nutrition, lifestyle, exercise, and supplements.
Overall, the book gives the reader more or less the right information. Right away I could tell that Owens has been highly influenced by Diana Schwarzbein, Paul Chek, Charles Poliquin and others that are pretty knowledgeable. These authors all generally believe that health is something that is hormonally determined, and that the best way to optimize the hormonal environment is through quality nutrition, a low-stress lifestyle with the right attitude, “smart” exercise meaning a preference for resistance training over endurance exercise, and supplements if needed.
With a foundation like that, the information in the book is more or less solid and can only stray so far from guidelines of the highest importance.
Of course the book has a pronounced low-carb bias due to such influences, which in the modern world probably does tend to outperform high-carb diets knowing that your average American receives 1,100 daily calories from a combined total of refined sweeteners and white flour. A low-carb diet eliminates this catastrophic problem, and is automatically superior – especially in the short-term. But there were definitely some one-liners in there about “too many carbohydrates” as if carbohydrates were somehow the enemy. If I’ve discovered anything about carbohydrates it’s that shunning carbohydrates in general simply can’t compete with replacing “bad” carbohydrates with “good” carbohydrates – which I view as more of an antidote to the problems caused by excess refined carbohydrate consumption.
But Owens is still clearly not an extremist by any stretch, and doesn’t deserve to be raked over any coals for her low-carb bias as it is VERY slight.
Rather, Owens should be truly commended for her excellent exercise information. Owens has several personal training certificates and it’s more than obvious that this is her area of expertise. Just as with Cosgrove, the exercise segment is by far the highlight. Some quotes from her chapter on reducing “LSD,” or long, slow, distance training, are truly legendary. For creating an optimal hormonal environment for both physique enhancement, metabolism, and functional longevity, I couldn’t agree more that short, hard training and resistance exercise and avoidance of LSD is the ticket. Paula’s ripped female figure is strong testimony to that.
p. 193
"One must exercise for long duration and often in order to burn any amount of fat with LSD. This is how long distance runners maintain their slim physiques. However, when a runner sustains an injury and is unable to train their metabolism spirals down. This leads to increased body fat over time."
This has been my response to endurance exercise time and time and time and time and time again. Only when it exceeds 20 hours per week is the calorie burn so high that fat has no choice but to leave your body. This exercise is very hard on the body, it causes muscle loss and a huge drop in metabolism (sends my basal temp. to the low-96’s), and results in a higher ratio of body fat to lean mass the MOMENT that you stop doing it – which you likely will due to injury, illness, or burnout.
p. 197
"LSD exercise is problematic because it causes cortisol to rise unopposed by the growth-promoting hormones, testosterone and growth hormone. This creates a physical stress response to your entire body. Prolonged release of cortisol, whether from long-term physical mental, or emotional stress, or the wrong kind of exercise, atrophies your muscles, nerves and brain cells. This may explain why standard aerobic exercise is not effective for optimal body composition and why marathon runners exhibit frail bodies devoid of muscle. The duration - not the intensity - of the exercise is the most significant issue in regards to cortisol. Chronic over-secretion of cortisol causes a weakened immune system, a decrease in lean muscle, hair loss, thinning skin, infertility, inability to grow nails and a decrease in concentration and memory. Excess cortisol kills brain cells, including those in the hippocampus, where the brain processes emotions. Excessive cortisol production can also deplete serotonin levels causing depression."
This quote is pure genius, and after the Thanksgiving holiday I hope we get a chance to dive straight into the diametrically-opposed functions of cortisol and testosterone – and how this is a prime determinant of how you age, your body composition, your immune system, athletic ability, and more. BTW Scott Abel's blog post on holiday eating is out of this world. Read it HERE.
So yes, overall Paula’s book is great. The exercise segment is remarkable and spot on. Now time for some negative criticisms…
Owens continually comes up with various lists of things to do in each category. While I wouldn’t disagree with many of her bulleted items in terms of say, their validity, I think it is a huge error to give your average person multiple lists of almost jaw-dropping length to focus on for health. Her list on lifestyle, for example, would be much better if she picked the top 4 most important things for people to focus on. Instead, the list, I kid you not, contains over 50 To-do’s, and includes nebulous and distracting things like:
“Refrain from judgment” and “Journal your thoughts.”
Her list in the nutrition category is even longer and puts the same emphasis, due to the nature of her lengthy bulleted lists, on including “more green drinks to create alkalinity” and eliminating “refined sugar.” Clearly there needs to be a little more prioritization going on there.
Of course, most of her bulleted items aren’t even discussed in detail. Several things that you are supposed to do would require a book on why you should do that. Lists of “do this, don’t do that” without any explanation or reasoning as to why doesn’t sit well with me, and I can’t see such things making any kind of impact on a real person in the real world. Rather it obscures the few basic things that really do make a difference with a bunch of nebulous, paranoid, distracting stuff that really doesn’t.
While Paula may have some powerful know how and knowledge that she is eager to share, her strategy for writing this book was not very well thought out. She shared far too much with too little to back it up.
There were also some unbelievably odd and off-base statements made here and there. They really threw me off. For example:
p. 40
“Reducing your intake of sugar and refined grains, which are omega-6 fatty acids, will result in decreased triglycerides.”
What the huh?
p. 41
“Grain-fed beef, refined cereals and vegetable oils such as sunflower, safflower, corn and soybean are foods high in omega-6.”
Grain-fed beef and refined cereals are not high in omega 6. In fact, by weight, walnuts (something Paula likes and advocates eating even though she is anti omega 6), contain 116 times more omega 6 than grain fed ground beef sirloin (90% lean). And refined cereals have a lot LESS omega 6 than unrefined cereals.
Conclusion:
Overall, I get a great vibe from Paula. There’s no question that if you are a woman (or man) living near the Phoenix area where Paula resides and looking for someone to help you improve your health and get a body that you never thought possible, Paula is the FIRST person to call. I have no doubts that her 21-Day Program is a great place for anyone to start when it comes to improving their health and body composition.
The book itself is full of great information, clouded by Mercola-fication of having 327 things to address when getting healthy instead of something more realistic, and just not that well written (typical of many great minds in the fitness field who attempt to write books). I would never discourage anyone from reading it though, as all of it is on the right track and there’s no doubt that the lives of many will be positively influenced by the gems that reside in The Power of 4. Thank you Paula, for putting it out into the world and overflowing with your passion for health. There are many in need of guidance out there, and I can only assume from what I know of you thus far that you are one of the world’s best. Keep up the good work. And Paula, you are totally hot (like Gwyneth Paltrow without the macrobiotics-induced osteopenia). You don't need your dog in the picture to make you look good :) More from Paula at www.paulaowens.com
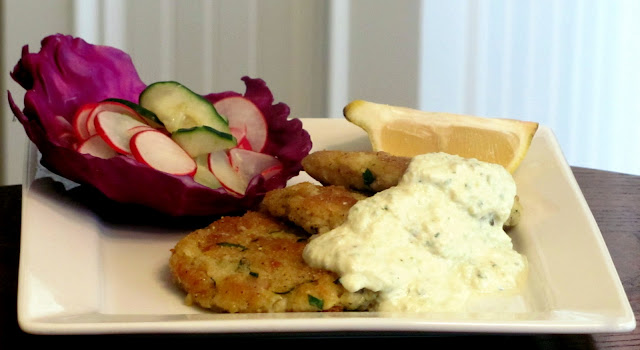
Pan-Fried Garbanzo-Millet Cakes with Sweet Vinaigrette Salad
 |
| The Health Seeker's Kitchen |
This meal idea came from a cookbook my daughter, Morgan, bought me for Mothers Day. I switched the recipes up, made my own pickled cucumbers and made a few changes on the ingredients. I am going to include the recipes with all the changes I made. The book for my inspiration is called Mayumi's Kitchen. I have also included recipes for Tofu Mayonnaise, Tofu Tarter Sauce, Pickled Cucumbers & the Sweet Vinaigrette Salad all with my recipe changes. This recipe makes 12 patties, so the next day I was able to make sandwiches with the tofu mayonnaise, romaine lettuce and the cakes (see picture below). These cakes are nutrition packed. One cup of garbanzo beans contain over 12 grams of fiber and 15 grams protein.
Millet acts as a prebiotic in the intestine to help feed the good bacteria that keep the intestines healthy, the immune system primed and it is naturally gluten free. It is also a good source of fiber, both soluble and insoluble, for heart and digestive health.
Dulse is extremely high in vitamins B6 and B12, as well as iron, potassium and fluoride. Dulse also contains a large shopping list of other vitamins and nutrients, including vitamins C, E, and A, magnesium, calcium, dietary fiber and protein. Additionally, dulse is a natural source of iodine, essential for thyroid gland health and thyroid hormone secretion. Rich with trace minerals from sea elements.
Pan-Fried Garbanzo-Millet Cakes
Printable Recipe Serves 4
1 15 oz. can organic garbanzo beans drained and mashed
2 tablespoons of Dulse dried leaves (Sea Vegetable)
1 cup millet, washed and drained
1/2 cup diced onion
3 Tbsp corn meal
1/4 cup finely chopped flat-leaf parsley
3 Tbsp. olive oil
sea salt & pepper to taste
lemon (sliced in wedges for serving)
1. Cook millet, dulse leaves and onions with 2 1/2 cups water. Break off dulse leaves and form into tablespoon for amount needed. Bring to a boil, then reduce heat to low and simmer for 30 minutes.
2. Mash garbanzo beans and then add millet, corn flour and parsley.
3. Form into 12 patties and cook in olive oil until well browned on both sides. Salt & pepper to taste as you cook. Serve with tofu tarter sauce, sweet vinaigrette salad & lemon wedge.
Tofu Mayonnaise
1 14 oz. soft tofu
3 Tbsp. apple cider vinegar
1 tbsp. raw agave nectar
4 tbsp. olive oil
1/2 tsp. salt
2 tsp. Dijon mustard
1.) Put ingredients in blender and blend until smooth. Be sure and use smooth or silken tofu. I used firm tofu and it was not as smooth as it should have been. Store in glass jar and use within 5 days.
Pickled Cucumber
1/2 heaping cup thinly sliced cucumber (with peels)
1/2 cup apple cider vinegar
1/2 tsp. salt
Mix together in bowl and let sit for 30 minutes.
Sweet Vinaigrette Salad
1 heaping cup thinly sliced radishes (with peels)
1 heaping cup thinly sliced cucumbers (with peels)
1/4 tsp. sea salt
1/2 cup apple cider vinegar
2 tbsp. raw agave nectar
red cabbage leaves
1 tbsp. sesame seeds (optional)
1. Place cucumbers, radishes and salt in a small mixing bowl. Place a plate for weight directly on the vegetables to smash them down in the bowl. Let sit for 25 minutes. Drain liquid and prepare vinaigrette dressing.
2. Make vinaigrette by placing apple cider vinegar and agave nectar together.
3. Toss vegetables with 1/4 cup of the vinaigrette dressing. Serve on top of purple cabbage leaves and sprinkle with sesame seeds.
Tofu Tarter Sauce
1 cup Tofu Mayonnaise
4 tbsp. almond milk
1/3 cup pickled cucumber (recipe above)
1 tsp. minced garlic
Place all ingredients in blender and blend until smooth. Serve on top or in a separate small serving bowl with the Garbanzo-Millet Cakes.
 |
| Garbanzo-Millet Sandwiches on Sprouted Wheat Bread The Health Seeker's Kitchen |
 |
| The Health Seeker's Kitchen |
Thursday, 18 November 2010
GABA Neurons and Rett Syndrome
Rett Syndrome is a rare (1 in every 10,000 to 15,000 live female births) neurodevelopmental disorder that occurs almost exclusively in young girls. This syndrome shares features with autism. The disorder is caused by a mutation of the MECP2 (methyl-CpG-binding protein 2) gene (MECP2 translation protein diagram noted on the right). This gene is found on the X chromosome. Infant boys born with the mutation typically die shortly after birth as they have no reserve X chromosome that may compensate to a degree with the mutation.
Rett Syndrome is typically diagnosed in early childhood when the following essential diagnostic criteria are met:
A recent study published in Nature examined a potential mechanism to explain some of the stereotypical behaviors found in Rett Syndrome. Using a mouse model, mice were produced that lacked MeCP2 in the brain gamma amino butryic acid (GABA) neurons. These mice demonstrated a series of neurobehavioral abnormalities similar to Rett syndrome including: repetitive behavior, impaired motor coordination, social interaction abnormalites and reduced startle response. These mice showed evidence of significant reduction in GABA content in the brain cortex and striatum regions.
The authors note their study "demonstrate(s) that GABAergic dysfunction is a critical mediator of Rett syndrome phenotypes". They note that MeCP2 mutations are found in a relatively rare number of humans with bipolar disorder, schizophrenia and autism. They note that GABAergic dysregulation through a variety of mechanisms may be central to these neuropsychiatric disorders.
If you are interested in learning more about the features of Rett Sydrome, I embedded theYouTube video below that documents the developmental history of Chelsea--an 11 year old girl with Rett Syndrome.
Further information on Rett Syndrome at the International Rett Syndrome Association website as well as from a Fact Sheet on Rett Syndrome from the National Institute of Neurological Disorders and Stroke.
Diagram of MECP2 protein is licensed under the Creative Commons Attribution Share Alike 3.0 unported license with author Emw.
Chao, H., Chen, H., Samaco, R., Xue, M., Chahrour, M., Yoo, J., Neul, J., Gong, S., Lu, H., Heintz, N., Ekker, M., Rubenstein, J., Noebels, J., Rosenmund, C., & Zoghbi, H. (2010). Dysfunction in GABA signalling mediates autism-like stereotypies and Rett syndrome phenotypes Nature, 468 (7321), 263-269 DOI: 10.1038/nature09582
Rett Syndrome is typically diagnosed in early childhood when the following essential diagnostic criteria are met:
- Normal development until 6 to 18 months of age
- Normal head circumference at birth followed by a slowing of the rate of head growth between 3 months and 4 years of age
- Severe impairment in expressive language
- Repetitive and stereotypic hand movements
- Gait abnormalities--toe walking or wide-based, stiff-legged walk
A recent study published in Nature examined a potential mechanism to explain some of the stereotypical behaviors found in Rett Syndrome. Using a mouse model, mice were produced that lacked MeCP2 in the brain gamma amino butryic acid (GABA) neurons. These mice demonstrated a series of neurobehavioral abnormalities similar to Rett syndrome including: repetitive behavior, impaired motor coordination, social interaction abnormalites and reduced startle response. These mice showed evidence of significant reduction in GABA content in the brain cortex and striatum regions.
The authors note their study "demonstrate(s) that GABAergic dysfunction is a critical mediator of Rett syndrome phenotypes". They note that MeCP2 mutations are found in a relatively rare number of humans with bipolar disorder, schizophrenia and autism. They note that GABAergic dysregulation through a variety of mechanisms may be central to these neuropsychiatric disorders.
If you are interested in learning more about the features of Rett Sydrome, I embedded theYouTube video below that documents the developmental history of Chelsea--an 11 year old girl with Rett Syndrome.
Further information on Rett Syndrome at the International Rett Syndrome Association website as well as from a Fact Sheet on Rett Syndrome from the National Institute of Neurological Disorders and Stroke.
Diagram of MECP2 protein is licensed under the Creative Commons Attribution Share Alike 3.0 unported license with author Emw.
Chao, H., Chen, H., Samaco, R., Xue, M., Chahrour, M., Yoo, J., Neul, J., Gong, S., Lu, H., Heintz, N., Ekker, M., Rubenstein, J., Noebels, J., Rosenmund, C., & Zoghbi, H. (2010). Dysfunction in GABA signalling mediates autism-like stereotypies and Rett syndrome phenotypes Nature, 468 (7321), 263-269 DOI: 10.1038/nature09582
Beefless Veggie Stir-Fry
This is a delicious and easy meal that you can whip up quickly with items you always have on hand. My taste-testers said it was very yummy as they cleaned their plates:) You can serve this with a big salad and my Perfect Brown Rice recipe below. You can also make this with 1/2 the package of beefless tips and add more of your favorite vegetables. It would be delicious with snow peas and water chestnuts. You can also spice it up by adding some hot peppers.
Beefless Veggie Stir-Fry
Printable Recipe
Marinade:
1 9oz. package gardein home style beefless tips
1 tbsp. olive oil
3 large minced garlic cloves
1 tsp. raw sugar
1/2 tsp. salt
1/8 tsp. pepper
Sauce:
1/4 cup apple cider vinegar
2 tsp raw cane sugar
2 tbsp. orange juice
5 tbsp. Nama Shoyu (soy sauce) or Bragg's Liquid Aminos
1 tbsp. arrowroot powder
2 tbsp. water
Vegetables:
2 carrots sliced
1 small onion
1/2 red bell pepper
handful of cilantro
1. Marinate beefless tips in olive oil, garlic, sugar, salt & pepper for 15 -20 minutes.
2. Place in wok or pan and stir fry until lightly browned on all sides.
3. Add sauce to beefless tips and cook for 1 minute.
4. Add vegetables and cook another 3 minutes.
5. Mix arrowroot powder and water together. Add to stir fry and stir until liquid is thickened.
6. Serve with Perfect Brown Rice.
7. Garnish with extra cilantro on side.
Perfect Brown Rice
1 cup uncooked brown rice
1 tsp. olive oil
2 cups filtered water
1. Fix brown rice by cooking in 1 tsp. olive oil until lightly browned. Add 2 cups water all at once. Quickly put on lid and bring to boil. Turn down heat to simmer until all water has evaporated (around 40 minutes).
Beefless Veggie Stir-Fry
Printable Recipe
Marinade:
1 9oz. package gardein home style beefless tips
1 tbsp. olive oil
3 large minced garlic cloves
1 tsp. raw sugar
1/2 tsp. salt
1/8 tsp. pepper
Sauce:
1/4 cup apple cider vinegar
2 tsp raw cane sugar
2 tbsp. orange juice
5 tbsp. Nama Shoyu (soy sauce) or Bragg's Liquid Aminos
1 tbsp. arrowroot powder
2 tbsp. water
Vegetables:
2 carrots sliced
1 small onion
1/2 red bell pepper
handful of cilantro
1. Marinate beefless tips in olive oil, garlic, sugar, salt & pepper for 15 -20 minutes.
2. Place in wok or pan and stir fry until lightly browned on all sides.
3. Add sauce to beefless tips and cook for 1 minute.
4. Add vegetables and cook another 3 minutes.
5. Mix arrowroot powder and water together. Add to stir fry and stir until liquid is thickened.
6. Serve with Perfect Brown Rice.
7. Garnish with extra cilantro on side.
Perfect Brown Rice
1 cup uncooked brown rice
1 tsp. olive oil
2 cups filtered water
1. Fix brown rice by cooking in 1 tsp. olive oil until lightly browned. Add 2 cups water all at once. Quickly put on lid and bring to boil. Turn down heat to simmer until all water has evaporated (around 40 minutes).
Wednesday, 17 November 2010
Overfeeding Reduces Insulin Resistance?
I had to laugh as the Mayor of Hair Danny Roddy contacted me, wondering if I had heard what was being said about me at this year’s Weston A. Price Foundation conference this past weekend. I had not, but I followed his lead and snooped around on Twitter where there was a tidbit about Stephan Guyenet being asked about overfeeding reducing insulin resistance.
“Ah, you’ve been reading Matt Stone,” he said, or something along those lines. “Overfeeding does NOT decrease insulin resistance. I don’t know where he got that idea from.”
Well, I figured this was a good opportunity to share exactly where I got that idea from, and why I believe it to be so as it is defined here.
First of all, “overfeeding” is a misnomer and I should probably stop using it. Overfeeding, in the medical literature, means giving someone a closely-monitored increase in calories above their normal, weight-maintenance requirement. When people embark upon RRARF, my program that you can read about in a Free eBook HERE, calories are not monitored. Rather, one is asked to eat at least to the satisfaction of the natural appetite and perhaps a little BEYOND appetite. I don’t say to force feed, but explicitly say to “eat as much as you can ENJOY.”
For many, this may equate to overfeeding. For others, maybe not. When eating an exclusively whole foods diet, particularly when switching out fibrous starchy foods for refined sugar and eating foods with no flavor enhancers, calorie consumption often spontaneously decreases. Although I would say that cases in which people lose weight doing RRARF is an indicator that calorie consumption decreased, I’ve also found this to be untrue – as one person in particular reported increasing calorie intake from 1,000 per day to 2,200-2,500 per day and losing 14 pounds in 2 months time. It is unpredictable, and since all the factors relevant to weight loss, calorie consumption, insulin sensitivity, and so on are not measured – no real verifiable conclusions can be made.
But I’m not Walter Willett, and I cannot have whatever I could possibly dream up to do a study on actually be sponsored and take place. I must resort to monitoring what actually happens to people when they follow this advice.
So is RRARF overfeeding? Who cares. It’s the unrealistic fiber-free fructose and corn oil-laden studies on overfeeding (a good way to develop hepatic insulin resistance like Morgan Spurlock did) that are irrelevant, not the real-life experiences and health impacts that people have who are trying the recommendations I’ve laid out in RRARF based on my own research, theories, experimentation, and personal observation.
Anyway, let’s back up a moment. I first got the idea that eating MORE food could reconcile insulin resistance while reading Schwarzbein’s books. In those books, it’s not necessarily insulin being spiked by high-calorie loads, fat interfering with glucose uptake, or carbohydrates that cause resistance to insulin. In fact, Schwarzbein goes on and on about how cortisol, elevated by things such as undereating, undersleeping, or overexercising (all things addressed as part of RRARF), can be a player in the development of metabolic syndrome. She states, explicitly for those with insulin resistance and weight problems, that they should be “eating more food, more often.”
Once again, since Schwarzbein is a practicing endocrinologist, she was actually able to see how this advice performs on basic tests such as glucose tolerance, cortisol levels, insulin levels, and so forth. Real experience and real observation with real people living in the real world.
This idea was greatly strengthened when I read Russ Farris and Per Marin’s The Potbelly Syndrome. I consider these two gentlemen to be some of the finest researchers out there. The book of course was about the hormone cortisol and contained the following passage:
“…insulin resistance leads to weight gain, but most health professionals believe that the opposite is true. If obesity does cause insulin resistance, then we would expect people who are overfed to become more insulin resistant, but that is not the case. Researchers in Indianapolis overfed six slender, active, young adults for several weeks… Five of the six subjects became LESS insulin resistant!”
This made perfect sense to me as I had been studying the wacky world of obesity research at the time, and overfeeding resulted in a drop in hunger, a rise in metabolism, and difficulty gaining more fat the more fat subjects gained. In other words, overfeeding brought about the triggering of mechanisms that made the body work hard AGAINST fat gain, and induce fat loss. Doesn’t sound like what I know of insulin resistance, which suggests that insulin resistance leads to hunger, reduced metabolism, increased propensity to store fat, and so forth.
Likewise, with underfeeding as in Ancel Keys’s The Biology of Human Starvation, underfeeding made the men ravenously hungry, store fat at an incredible rate – particularly in the abdominal region indicative of insulin resistance, without building back muscle tissue, and other signs of insulin resistance, not sensitivity. Only after binge eating on pies, pastries, and dairy products up to 7,000 calories per day and gaining a ton of body fat did they rebuild their lost muscle mass and start to spontaneously lose body fat at an amazing rate (while still continuing to gain lean mass) eating to appetite.
In other words, underfeeding made them gain belly fat eating to appetite. Overfeeding made them lose belly fat eating to appetite. It’s not really that wild of a concept, and knowing how well the human body defends against a shift away from its weight set point, it should be no surprise that gaining weight via overfeeding causes the body to become more insulin sensitive, which increases muscle building and heat production, minimizes fat storage even in the face of massive calorie intakes as was witnessed in the famous Ethan Sims overfeeding study, while decreasing appetite.
Anyway, overfeeding lowers cortisol just as underfeeding raises it. The effects of overfeeding and underfeeding mirror one another. Even a book as scientifically straightforward as Lyle McDonald’s Ultimate Diet 2.0 lays out a simple chart of hormonal changes that take place during overfeeding vs. underfeeding. Underfeeding increases cortisol. Overfeeding decreases it.
This is the presumed mechanism, considering that cortisol blocks the action of insulin and leptin for that matter which is even more significant (and probably why underfeeding causes the weight set point to rise), that makes changes in weight a negative feedback system. This was the whole point of Russ Farris and Per Marin’s book, which can be summarized as: “Hypercortisolism causes insulin resistance, dummy, not carbs or eating too much.”
Overall the best sign of improved insulin sensitivity is improved glucose clearance from the blood after eating. I was so captivated by overfeeding’s potential surprise ability to improve insulin resistance, that I tried RRARF while monitoring my blood glucose levels and found my postprandial blood glucose readings to drop by more than 25% after just 30 days. Even two baked potatoes at a 1,000+ calorie feast couldn’t send my blood sugar above 75 mg/dl by the end of it, and I gained abdominal fat in the process, which is even more out of synch with the misinterpretations of the scientific literature held by most researchers.
Of course, many of you that have gone through the rigors of testing your own blood glucose levels witnessed the same thing while eating beyond appetite of whole foods. Martin, Lisa, Sheri and her husband, and Undertow come to mind. Sheri for example, writes:
"My temps are great going from 96.4 up to 97.8 and even 98.0 on some days. During ovulation I was 98.5-98.7. My fasting glucose started in the low 100’s and has only dropped to a consistent 93, better but I still obviously need it lower. Then my 1 hour postprandial glucose reading jumps all over from 199 at first and then on different days 140’s or 150’s. It has been in the 110’s and low 120’s lately and I get excited it’s improving but then will jump up to the 140’s again. I sleep a million times better, have less joint pain from an autoimmune disease and didn’t have cramps during my period for the first time in years. I have gained 5 unwanted pounds but oh well. My husband has increased his temps from 95.9 to between 97.0 - 97.5 depending on the day and also sleeps a million times better. Poor thing really packed it on with a whopping .2 pound gain- not even a half a pound. His fasting glucose has stayed even at around 87. His postprandial glucose readings have gone from the 120’s and 130’s to a typical 103. We have nothing negative to say about our experience so far and are very thankful to you, Matt."
I also just received some harder data from Chris Sandel of www.seven-health.com/
You can and read about him here: http://www.seven-health.com/about-us/
I went through his extensive data, and there is no question that his glucose clearance improved during the 30 some odd days he spent doing RRARF. To get some figures, I went through his data and did some averaging. I compared the readings from the first half of his month on RRARF to the 2nd half of his month on RRARF, and took averages and compared them. Here are the changes:
Weight Increase: 0.4 kg (insignificant)
Basal body temperature increase: Very slight from 35.81 C to 35.98 C
Fasting glucose: -4.6% from 98 mg/dl to 93 mg/dl
1-Hour postprandial glucose: -10.5% from 115 mg/dl to 103 mg/dl
2-Hour postprandial glucose: -10.9% from 119 mg/dl to 106 mg/dl
It’s also of interest that his highest 2-hour postprandial reading, which I view to be the most significant, was typically higher, and sometimes much higher than his 1-hour postprandial test towards the beginning of the experiment. This is an almost sure sign of impaired glucose metabolism, but all in all his numbers are decent for an endurance athlete taking a break (which as I’ve described in the past, from my own experience, as being a tough transition).
By the end he was able to reverse that on most days, but still has a little way to go before it’s perfected.
His highest 2-hour postprandial test was on days #9 and #10 of the experiment, which is probably pretty typical. On both of those days, his 2-hour reading was 135 mg/dl.
His lowest reading was on Day 30 of the experiment at a mere 97 mg/dl – roughly the same as his fasting level at the beginning of the experiment.
So that’s that. Maybe you can’t pinpoint what I’m talking about in the medical literature. Maybe what I’m saying doesn’t make sense with everything you’ve studied or been led to believe. Maybe you view this as poorly-controlled information (which it is) and thus unscientific and irrelevant.
But this is real and is really happening in the real world to real people, which, at the end of the day, is what really counts. Former extreme tater-hater 180-Katie summed it up best when she wrote to me:
“Finally, my blood sugar control is better. A lot better! I have no idea why eating starch would improve my blood sugar control like this, but it does. It could be elf magic or nanobots for all I care, it works!”
“Ah, you’ve been reading Matt Stone,” he said, or something along those lines. “Overfeeding does NOT decrease insulin resistance. I don’t know where he got that idea from.”
Well, I figured this was a good opportunity to share exactly where I got that idea from, and why I believe it to be so as it is defined here.
First of all, “overfeeding” is a misnomer and I should probably stop using it. Overfeeding, in the medical literature, means giving someone a closely-monitored increase in calories above their normal, weight-maintenance requirement. When people embark upon RRARF, my program that you can read about in a Free eBook HERE, calories are not monitored. Rather, one is asked to eat at least to the satisfaction of the natural appetite and perhaps a little BEYOND appetite. I don’t say to force feed, but explicitly say to “eat as much as you can ENJOY.”
For many, this may equate to overfeeding. For others, maybe not. When eating an exclusively whole foods diet, particularly when switching out fibrous starchy foods for refined sugar and eating foods with no flavor enhancers, calorie consumption often spontaneously decreases. Although I would say that cases in which people lose weight doing RRARF is an indicator that calorie consumption decreased, I’ve also found this to be untrue – as one person in particular reported increasing calorie intake from 1,000 per day to 2,200-2,500 per day and losing 14 pounds in 2 months time. It is unpredictable, and since all the factors relevant to weight loss, calorie consumption, insulin sensitivity, and so on are not measured – no real verifiable conclusions can be made.
But I’m not Walter Willett, and I cannot have whatever I could possibly dream up to do a study on actually be sponsored and take place. I must resort to monitoring what actually happens to people when they follow this advice.
So is RRARF overfeeding? Who cares. It’s the unrealistic fiber-free fructose and corn oil-laden studies on overfeeding (a good way to develop hepatic insulin resistance like Morgan Spurlock did) that are irrelevant, not the real-life experiences and health impacts that people have who are trying the recommendations I’ve laid out in RRARF based on my own research, theories, experimentation, and personal observation.
Anyway, let’s back up a moment. I first got the idea that eating MORE food could reconcile insulin resistance while reading Schwarzbein’s books. In those books, it’s not necessarily insulin being spiked by high-calorie loads, fat interfering with glucose uptake, or carbohydrates that cause resistance to insulin. In fact, Schwarzbein goes on and on about how cortisol, elevated by things such as undereating, undersleeping, or overexercising (all things addressed as part of RRARF), can be a player in the development of metabolic syndrome. She states, explicitly for those with insulin resistance and weight problems, that they should be “eating more food, more often.”
Once again, since Schwarzbein is a practicing endocrinologist, she was actually able to see how this advice performs on basic tests such as glucose tolerance, cortisol levels, insulin levels, and so forth. Real experience and real observation with real people living in the real world.
This idea was greatly strengthened when I read Russ Farris and Per Marin’s The Potbelly Syndrome. I consider these two gentlemen to be some of the finest researchers out there. The book of course was about the hormone cortisol and contained the following passage:
“…insulin resistance leads to weight gain, but most health professionals believe that the opposite is true. If obesity does cause insulin resistance, then we would expect people who are overfed to become more insulin resistant, but that is not the case. Researchers in Indianapolis overfed six slender, active, young adults for several weeks… Five of the six subjects became LESS insulin resistant!”
This made perfect sense to me as I had been studying the wacky world of obesity research at the time, and overfeeding resulted in a drop in hunger, a rise in metabolism, and difficulty gaining more fat the more fat subjects gained. In other words, overfeeding brought about the triggering of mechanisms that made the body work hard AGAINST fat gain, and induce fat loss. Doesn’t sound like what I know of insulin resistance, which suggests that insulin resistance leads to hunger, reduced metabolism, increased propensity to store fat, and so forth.
Likewise, with underfeeding as in Ancel Keys’s The Biology of Human Starvation, underfeeding made the men ravenously hungry, store fat at an incredible rate – particularly in the abdominal region indicative of insulin resistance, without building back muscle tissue, and other signs of insulin resistance, not sensitivity. Only after binge eating on pies, pastries, and dairy products up to 7,000 calories per day and gaining a ton of body fat did they rebuild their lost muscle mass and start to spontaneously lose body fat at an amazing rate (while still continuing to gain lean mass) eating to appetite.
In other words, underfeeding made them gain belly fat eating to appetite. Overfeeding made them lose belly fat eating to appetite. It’s not really that wild of a concept, and knowing how well the human body defends against a shift away from its weight set point, it should be no surprise that gaining weight via overfeeding causes the body to become more insulin sensitive, which increases muscle building and heat production, minimizes fat storage even in the face of massive calorie intakes as was witnessed in the famous Ethan Sims overfeeding study, while decreasing appetite.
Anyway, overfeeding lowers cortisol just as underfeeding raises it. The effects of overfeeding and underfeeding mirror one another. Even a book as scientifically straightforward as Lyle McDonald’s Ultimate Diet 2.0 lays out a simple chart of hormonal changes that take place during overfeeding vs. underfeeding. Underfeeding increases cortisol. Overfeeding decreases it.
This is the presumed mechanism, considering that cortisol blocks the action of insulin and leptin for that matter which is even more significant (and probably why underfeeding causes the weight set point to rise), that makes changes in weight a negative feedback system. This was the whole point of Russ Farris and Per Marin’s book, which can be summarized as: “Hypercortisolism causes insulin resistance, dummy, not carbs or eating too much.”
Overall the best sign of improved insulin sensitivity is improved glucose clearance from the blood after eating. I was so captivated by overfeeding’s potential surprise ability to improve insulin resistance, that I tried RRARF while monitoring my blood glucose levels and found my postprandial blood glucose readings to drop by more than 25% after just 30 days. Even two baked potatoes at a 1,000+ calorie feast couldn’t send my blood sugar above 75 mg/dl by the end of it, and I gained abdominal fat in the process, which is even more out of synch with the misinterpretations of the scientific literature held by most researchers.
Of course, many of you that have gone through the rigors of testing your own blood glucose levels witnessed the same thing while eating beyond appetite of whole foods. Martin, Lisa, Sheri and her husband, and Undertow come to mind. Sheri for example, writes:
"My temps are great going from 96.4 up to 97.8 and even 98.0 on some days. During ovulation I was 98.5-98.7. My fasting glucose started in the low 100’s and has only dropped to a consistent 93, better but I still obviously need it lower. Then my 1 hour postprandial glucose reading jumps all over from 199 at first and then on different days 140’s or 150’s. It has been in the 110’s and low 120’s lately and I get excited it’s improving but then will jump up to the 140’s again. I sleep a million times better, have less joint pain from an autoimmune disease and didn’t have cramps during my period for the first time in years. I have gained 5 unwanted pounds but oh well. My husband has increased his temps from 95.9 to between 97.0 - 97.5 depending on the day and also sleeps a million times better. Poor thing really packed it on with a whopping .2 pound gain- not even a half a pound. His fasting glucose has stayed even at around 87. His postprandial glucose readings have gone from the 120’s and 130’s to a typical 103. We have nothing negative to say about our experience so far and are very thankful to you, Matt."
I also just received some harder data from Chris Sandel of www.seven-health.com/
You can and read about him here: http://www.seven-health.com/about-us/
I went through his extensive data, and there is no question that his glucose clearance improved during the 30 some odd days he spent doing RRARF. To get some figures, I went through his data and did some averaging. I compared the readings from the first half of his month on RRARF to the 2nd half of his month on RRARF, and took averages and compared them. Here are the changes:
Weight Increase: 0.4 kg (insignificant)
Basal body temperature increase: Very slight from 35.81 C to 35.98 C
Fasting glucose: -4.6% from 98 mg/dl to 93 mg/dl
1-Hour postprandial glucose: -10.5% from 115 mg/dl to 103 mg/dl
2-Hour postprandial glucose: -10.9% from 119 mg/dl to 106 mg/dl
It’s also of interest that his highest 2-hour postprandial reading, which I view to be the most significant, was typically higher, and sometimes much higher than his 1-hour postprandial test towards the beginning of the experiment. This is an almost sure sign of impaired glucose metabolism, but all in all his numbers are decent for an endurance athlete taking a break (which as I’ve described in the past, from my own experience, as being a tough transition).
By the end he was able to reverse that on most days, but still has a little way to go before it’s perfected.
His highest 2-hour postprandial test was on days #9 and #10 of the experiment, which is probably pretty typical. On both of those days, his 2-hour reading was 135 mg/dl.
His lowest reading was on Day 30 of the experiment at a mere 97 mg/dl – roughly the same as his fasting level at the beginning of the experiment.
So that’s that. Maybe you can’t pinpoint what I’m talking about in the medical literature. Maybe what I’m saying doesn’t make sense with everything you’ve studied or been led to believe. Maybe you view this as poorly-controlled information (which it is) and thus unscientific and irrelevant.
But this is real and is really happening in the real world to real people, which, at the end of the day, is what really counts. Former extreme tater-hater 180-Katie summed it up best when she wrote to me:
“Finally, my blood sugar control is better. A lot better! I have no idea why eating starch would improve my blood sugar control like this, but it does. It could be elf magic or nanobots for all I care, it works!”
Subscribe to:
Comments (Atom)

















